WALTHAM, Mass., Sept. 05, 2018 (GLOBE NEWSWIRE) — Histogenics Corporation (Histogenics) (Nasdaq: HSGX), a leader in the development of restorative cell therapies that may offer rapid-onset pain relief and restored function, today announced that its Phase 3 clinical trial of NeoCart did not meet the primary endpoint of a statistically significant improvement in pain and function in a dual threshold responder analysis one year after treatment as compared to microfracture. In the modified Intent to Treat (mITT) population (which excludes those patients who were randomized but not treated with NeoCart), 74.2% of the NeoCart patients exhibited clinically meaningful improvements in pain and function compared to 62.0% of microfracture patients at one year (p=0.071). However, in this mITT population, patients treated with NeoCart achieved a statistically significant improvement in pain and function (p=0.018) six months after treatment as compared to patients treated with microfracture. Both NeoCart and microfracture were well tolerated and exhibited strong safety profiles.
“Based on the totality of the data generated in the Phase 3 clinical trial, we continue to believe in NeoCart’s potential as a treatment for knee cartilage damage. When we designed our Phase 3 clinical trial in 2009, we set a very high clinical bar for NeoCart and narrowly missed hitting the trial’s primary endpoint with statistical significance by only two microfracture responders out of the 249 patients that participated in the trial. While the NeoCart treatment group exhibited a response as early as three months after treatment that continued through two years, the microfracture response rate was better than expected, which impacted the statistics. We are encouraged by the results and believe we have a meaningfully differentiated product that, if approved, can compete effectively and provide physicians and patients with a beneficial treatment option that may grow the market,” said Adam Gridley, President and Chief Executive Officer of Histogenics. “We continue to analyze the data and are in the process of scheduling a meeting with the FDA to discuss the results and prepare for a potential submission of a biologics license application for NeoCart. We wish to acknowledge and thank the patients and investigators who participated in the trial and shared their positive experiences with NeoCart,” stated Mr. Gridley.
The NeoCart Phase 3 clinical trial is believed to be the largest and first prospectively designed, randomized clinical trial in North America evaluating the safety and efficacy of a restorative cell therapy to treat knee cartilage damage. It is also believed to be the only trial with a dual threshold responder analysis endpoint. As part of the prospective data analysis, Histogenics collected a variety of patient reported outcome endpoints, including all measures of the Knee Injury and Osteoarthritis Outcomes Score (KOOS) and the International Knee Documentation Committee (IKDC) score, which are validated, patient-centered assessments of pain and function that are commonly used in current clinical trials of cartilage therapies. On all but one of these measures, two of which are being utilized as primary endpoints in ongoing clinical trials by third parties in the U.S. for other therapies, NeoCart demonstrated statistically significant superiority versus microfracture at one and two years.
The Phase 3 clinical trial is the first study prospectively enrolled consistent with current U.S. Food and Drug Administration (FDA) guidance, which provides for the use of microfracture as a comparator treatment in trials to repair knee cartilage damage. The published FDA guidance also specifically calls for a study population that, given the clinical limitations and variable results of microfracture, we believe provides more favorable results than what is typically seen in microfracture in both the literature and a real-world setting.
“We are pleased with the overall performance of NeoCart in this Phase 3 clinical trial and the data confirm the feedback we have received from several of the investigators who participated in the trial. Most importantly, patients treated with NeoCart displayed an early and sustained recovery from pain and return to function that was clinically meaningful. The data from this trial are also consistent with results seen in prior clinical trials of NeoCart as well as the biomechanical data generated as part of our collaboration with Cornell University,” said Lynne Kelley, M.D., Chief Medical Officer of Histogenics. “While we are continuing to analyze the data, we have already seen a number of important results, including a statistically significant improvement of NeoCart compared to microfracture in lesion sizes of greater than 2 cm and patients with higher body mass index. We think that results such as these will be an important part of our planned discussions with the FDA, as well as with clinicians if NeoCart is approved,” continued Dr. Kelley.
There are approximately 1.2 million arthroscopic procedures conducted each year to treat knee cartilage defects in the U.S., with less than half of eligible patients currently electing to receive treatment. Based on the data generated to date, NeoCart may offer many of these patients a safe and effective alternative, subject to FDA approval.
“As a physician who treats patients with knee cartilage damage, I am keenly aware of the limitations of current treatment approaches for this common and underserved condition,” said David C. Flanigan, MD Associate Professor, Department of Orthopedics, Director, Cartilage Restoration Program at The Ohio State University Wexner Medical Center, and a high-enrolling investigator in the Phase 3 clinical trial. “The pain and loss of function associated with uncorrected knee cartilage lesions can significantly limit these patients’ ability to maintain their daily routines and often leads to other more serious comorbidities over time. The rapid recovery for patients who received this cartilage tissue implant compared to those who underwent microfracture indicates that implants, such as NeoCart, may be an attractive alternative for patients seeking a better quality of life and faster return to function,” continued Dr. Flanigan.
The primary endpoint for the Phase 3 clinical trial was a dual-threshold responder analysis measuring the improvement in KOOS pain and IKDC function scores for each patient treated with NeoCart compared to those treated with microfracture one year after the time of treatment. Dual-threshold responders were defined as patients who, relative to their baseline measurements, had at least a 12-point improvement in the KOOS pain sub-score assessment and a 20-point improvement in the IKDC subjective assessment. The trial also evaluated additional pain, quality of life, and function outcomes using all five measures of KOOS subscales, including Sports and Recreation. The change from baseline and the relative change between the NeoCart and microfracture arms was also measured at one year which contrasts with clinical trials of other products, either on the market or in development, that measured these changes at two years. Efficacy and safety will continue to be followed out to three years, and Histogenics expects to further track patients for future planned analyses, including patients from prior clinical trials who received a NeoCart treatment.
Demographics for both study arms were similar and represent a patient population that was intended to ensure that microfracture would respond favorably, including patients with an average age of approximately 39 years old and a Body Mass Index (BMI) of approximately 27. Furthermore, the mean lesion size was 2.1 cm in the NeoCart arm and 1.8 cm in the microfracture arm. There were no other significant differences between the treatment arms.
The results with respect to the primary endpoint (dual threshold responder analysis one year after treatment) are summarized below:
|
|
|
|
|
| |
NeoCart |
Microfracture |
|
|
| |
Positive
Responders |
Responder
Rate |
Positive
Responders |
Responder
Rate |
Difference |
|
| ITT |
121/170 |
71.2% |
49/79 |
62.0% |
9.2 |
p=0.1877 |
| mITT |
121/163 |
74.2% |
49/79 |
62.0% |
12.2 |
P=0.0714 |
| As Treated |
120/162 |
74.1% |
50/80 |
62.5% |
11.6 |
p=0.0735 |
| Per Protocol |
118/155 |
76.1% |
43/65 |
66.2% |
10.0 |
p=0.1362 |
|
|
|
|
|
|
|
Key additional findings from the clinical trial include:
NeoCart demonstrated statistically significant improvements in pain and function at both one and two years after treatment as measured by changes in the KOOS and IKDC scores.
|
| KOOS pain score (mITT Population) |
| Change from Baseline |
| (NeoCart Baseline = 54.0; Microfracture Baseline = 52.4) |
|
NeoCart |
Microfracture |
|
| Visit |
N |
Mean |
N |
Mean |
P-Value |
| 3-months |
160 |
24.1 |
75 |
22.4 |
0.0487* |
| 6-months |
157 |
28.6 |
75 |
27.0 |
0.0819 |
| 1-year |
158 |
31.4 |
72 |
28.7 |
0.0239* |
| 2-years |
87 |
32.2 |
34 |
28.9 |
0.0080* |
| 3-years |
39 |
34.3 |
16 |
30.7 |
0.1071 |
| * Statistically significant |
|
|
|
|
|
| IKDC subjective knee exam score (mITT Population) |
| Change from Baseline |
| (NeoCart Baseline = 40.3; Microfracture Baseline = 40.0) |
|
NeoCart |
Microfracture |
|
| Visit |
N |
Mean |
N |
Mean |
P-Value |
| 3-months |
159 |
13.7 |
76 |
14.5 |
0.9686 |
| 6-months |
156 |
24.4 |
74 |
22.4 |
0.1572 |
| 1-year |
158 |
33.1 |
71 |
28.3 |
0.0126* |
| 2-years |
87 |
35.3 |
34 |
30.2 |
0.0366* |
| 3-years |
38 |
39.9 |
16 |
32.6 |
0.2691 |
| * Statistically significant |
|
|
|
|
|
|
|
|
|
|
|
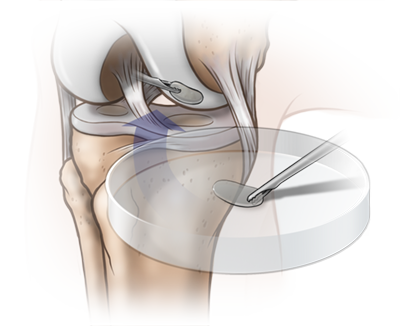
NeoCart, the most advanced therapy from Histogenics restorative cell therapy platform, is functional cartilage that combines breakthroughs in bio-engineering, biomaterials and cell processing to enhance the autologous cartilage repair process. NeoCart, which is one of the most rigorously studied restorative cell therapies for orthopedic use, merges a patient’s own cells with a fortified three-dimensional scaffold designed to accelerate healing and reduce pain. NeoCart’s ability to function like cartilage at the time of treatment may enable patients to return to work and daily activities more rapidly than currently available treatment options such as microfracture.
Histogenics is in the process of requesting a meeting with the FDA to discuss the data and a potential BLA submission. In addition, Histogenics intends to present the complete study results at upcoming medical conferences and will seek to have the data published in one or more peer reviewed journals.
Conference Call and Webcast Information
Histogenics management will host a conference call on Wednesday, September 5, 2018 at 8:30am EDT. A question-and-answer session will follow Histogenics’ remarks. To participate on the live call, please dial (877) 930-8064 (domestic) or (253) 336-8040 (international) and provide the conference ID 8764946 five to ten minutes before the start of the call.
To access a live audio webcast of the presentation on the “Investor Relations” page of the Histogenics website, please click here. A replay of the webcast will be archived on Histogenics’ website for approximately 60 days following the presentation.
About Histogenics Corporation
Histogenics (Nasdaq: HSGX) is a leader in the development of restorative cell therapies that may offer rapid-onset pain relief and restored function. Histogenics’ lead investigational product, NeoCart, is designed to rebuild a patient’s own knee cartilage to treat pain at the source and potentially prevent a patient’s progression to osteoarthritis. NeoCart is one of the most rigorously studied restorative cell therapies for orthopedic use. NeoCart is designed to perform like articular hyaline cartilage at the time of treatment, and as a result, may provide patients with more rapid pain relief and accelerated recovery as compared to the current standard of care. Histogenics’ technology platform has the potential to be used for a broad range of additional restorative cell therapy indications. For more information on Histogenics and NeoCart, please visit www.histogenics.com.
Forward-Looking Statements
Various statements in this release are “forward-looking statements” under the securities laws. Words such as, but not limited to, “anticipate,” “believe,” “can,” “could,” “expect,” “estimate,” “design,” “goal,” “intend,” “may,” “might,” “objective,” “plan,” “predict,” “project,” “target,” “likely,” “should,” “will,” and “would,” or the negative of these terms and similar expressions or words, identify forward-looking statements. Forward-looking statements are based upon current expectations that involve risks, changes in circumstances, assumptions and uncertainties.
Important factors that could cause actual results to differ materially from those reflected in Histogenics’ forward-looking statements include, among others: NeoCart’s potential as a treatment for knee cartilage damage; expectations regarding the timing and success of discussions with the FDA regarding the submission of a biologics license application for NeoCart; the timing, associated expenses and ability to obtain and maintain regulatory approval of NeoCart or any product candidates, and the labeling for any approved products; the market size and potential patient population in markets where Histogenics’ and its partners expect to compete; updated or refined data based on Histogenics’ continuing review and quality control analysis of clinical data; the scope, progress, timing, expansion, and costs of developing and commercializing Histogenics’ product candidates; the ability to obtain and maintain regulatory approval regarding the comparability of critical NeoCart raw materials following its technology transfer and manufacturing location transition; Histogenics’ expectations regarding its expenses and revenue; Histogenics’ ability to obtain additional debt or equity capital and other factors that are described in the “Risk Factors” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations” sections of Histogenics’ Annual Report on Form 10-K for the year ended December 31, 2017 and Quarterly Report on Form 10-Q for the quarter ended June 30, 2018, which are on file with the SEC and available on the SEC’s website at www.sec.gov. In addition to the risks described above and in Histogenics’ Annual Report on Form 10-K and Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and other filings with the SEC, other unknown or unpredictable factors also could affect Histogenics’ results.
There can be no assurance that the actual results or developments anticipated by Histogenics will be realized or, even if substantially realized, that they will have the expected consequences to, or effects on, Histogenics. Therefore, no assurance can be given that the outcomes stated in such forward-looking statements and estimates will be achieved.
All written and verbal forward-looking statements attributable to Histogenics or any person acting on its behalf are expressly qualified in their entirety by the cautionary statements contained or referred to herein. Histogenics cautions investors not to rely too heavily on the forward-looking statements Histogenics makes or that are made on its behalf. The information in this release is provided only as of the date of this release, and Histogenics undertakes no obligation, and specifically declines any obligation, to update or revise publicly any forward-looking statements, whether as a result of new information, future events or otherwise.
Contacts:
Investor Relations:
Tel: +1 (781) 547-7909
Media Relations:
Glenn Silver, Lazar Partners Ltd.
Tel: + 1 (646) 871-8485