CAMBRIDGE, Mass.–(BUSINESS WIRE)–InVivo Therapeutics Holdings Corp. (NVIV) today announced that the Foothills Medical Centre in Calgary, Alberta has been added as a Canadian clinical site for The INSPIRE Study: InVivo Study of Probable Benefit of theNeuro-Spinal Scaffold™ for Safety and Neurologic Recovery in Subjects with Complete Thoracic AIS A Spinal Cord Injury. The Foothills Medical Centre is the largest hospital in Alberta and is one of the most recognized medical facilities in Canada, providing advanced healthcare services to over two million people from Calgary and southern Alberta, the northwestern United States, southeastern British Columbia, and southern Saskatchewan.
“InVivo’s Neuro-Spinal Scaffold is one of the more innovative approaches to treating acute spinal cord injury in recent history and we look forward to being a part of the INSPIRE study,” said Steven Casha, M.D., Ph.D., Assistant Professor of Neurosurgery in the Department of Clinical Neurosciences and Principal Investigator at the study site.
Mark Perrin, InVivo’s CEO and Chairman, said, “We are pleased to welcome Dr. Casha and his team at the Foothills Medical Centre to the INSPIRE study. We will continue to expand our footprint in both the US and Canada.”
A new CEO’s Perspective discussing the current status of the INSPIRE study can be found on the InVivo Therapeutics website:http://www.invivotherapeutics.com/about-invivo/ceo-perspective/
There are now 24 clinical sites participating in the clinical study:
- Banner University Medical Center, Tucson, AZ
- Barnes-Jewish Hospital at Washington University Medical Center, St. Louis, MO
- Ben Taub Hospital/Baylor College of Medicine, Houston, TX
- Barrow Neurological Institute – St. Joseph’s Hospital and Medical Center, Phoenix, AZ
- Carolina Neurosurgery and Spine Associates/Carolinas Rehabilitation, Charlotte, NC
- Cooper Neurological Institute, Camden, NJ
- Foothills Medical Centre, Calgary, Alberta, Canada
- Goodman Campbell Brain and Spine/Indiana University Health Neuroscience Center, Indianapolis, IN
- Hospital of the University of Pennsylvania, Philadelphia, PA
- Keck Hospital of University of Southern California, Los Angeles, CA
- Medical College of Wisconsin/Froedtert Hospital, Milwaukee, WI
- Mount Sinai Hospital, New York, NY
- Northwestern Medicine, Chicago, IL
- Oregon Health & Science University, Portland, OR
- Rutgers New Jersey Medical School, Newark, NJ
- Thomas Jefferson University Hospital, Philadelphia, PA
- Toronto Western Hospital, Toronto, ON, Canada
- University of California, Davis Medical Center, Sacramento, CA
- University of California, San Diego Medical Center, San Diego, CA
- University of Kansas Medical Center, Kansas City, KS
- University of Louisville Hospital, Louisville, KY
- University of Pittsburgh Medical Center Presbyterian, Pittsburgh, PA
- University of Virginia Health System, Charlottesville, VA
- Vidant Medical Center, Greenville, NC
For more information, please visit the company’s ClinicalTrials.gov registration site: http://clinicaltrials.gov/ct2/show/study/NCT02138110
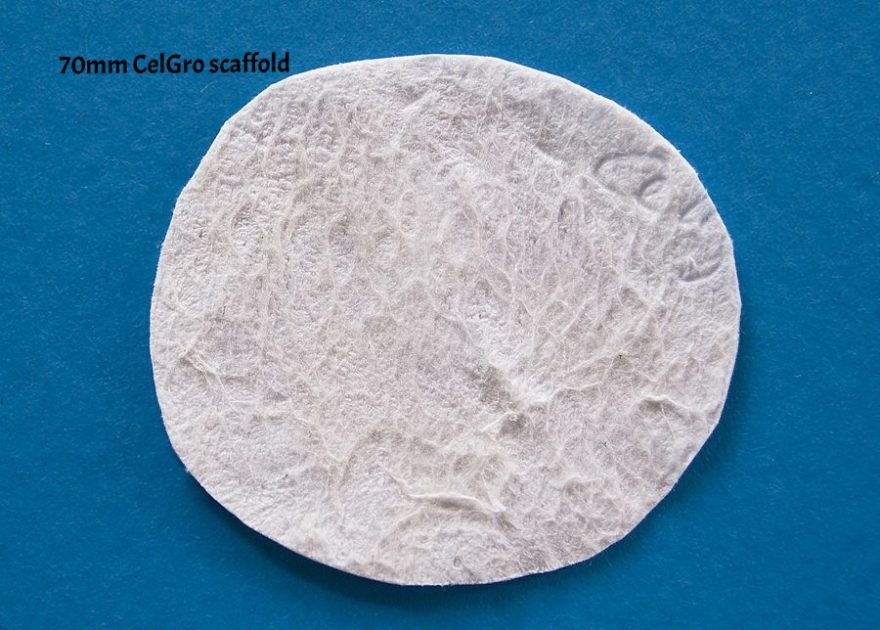
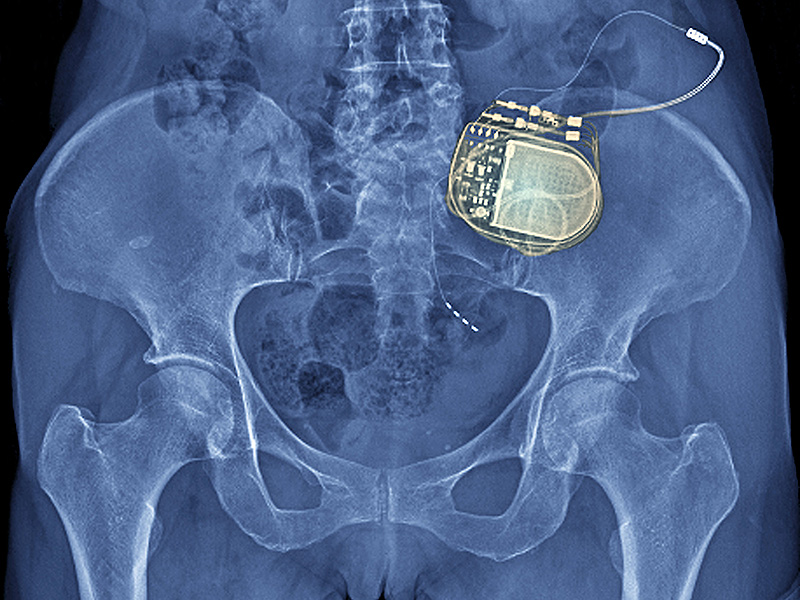
About the Neuro-Spinal Scaffold™ Implant
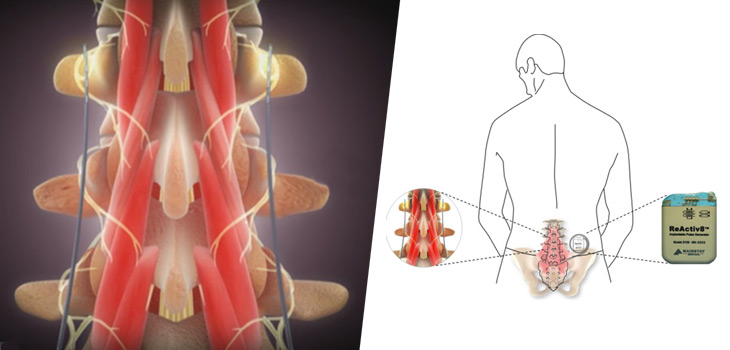
Following acute spinal cord injury, surgical implantation of the biodegradable Neuro-Spinal Scaffold within the decompressed and debrided injury epicenter is intended to support appositional healing, thereby reducing post-traumatic cavity formation, sparing white matter, and allowing neural regeneration across the healed wound epicenter. The Neuro-Spinal Scaffold, an investigational device, has received a Humanitarian Use Device (HUD) designation and currently is being evaluated in the INSPIRE pivotal probable benefit study for the treatment of patients with complete (AIS A) traumatic acute spinal cord injury.
About InVivo Therapeutics
InVivo Therapeutics Holdings Corp. is a research and clinical-stage biomaterials and biotechnology company with a focus on treatment of spinal cord injuries. The company was founded in 2005 with proprietary technology co-invented by Robert Langer, Sc.D., Professor at Massachusetts Institute of Technology, and Joseph P. Vacanti, M.D., who then was at Boston Children’s Hospital and who now is affiliated with Massachusetts General Hospital. In 2011, the company earned the David S. Apple Award from the American Spinal Injury Association for its outstanding contribution to spinal cord injury medicine. In 2015, the company’s investigational Neuro-Spinal Scaffoldreceived the 2015 Becker’s Healthcare Spine Device Award. The publicly-traded company is headquartered in Cambridge, MA. For more details, visit www.invivotherapeutics.com.
Safe Harbor Statement
Any statements contained in this press release or the CEO Perspective referred to herein that do not describe historical facts may constitute forward-looking statements within the meaning of the federal securities laws. These statements can be identified by words such as “believe,” “anticipate,” “intend,” “estimate,” “will,” “may,” “should,” “expect,” “designed to,” “potentially,” and similar expressions, and include statements regarding the safety and effectiveness of the Neuro-Spinal Scaffold, the expected timing of full enrollment in the INSPIRE study, the timing of the submission of the Humanitarian Device Exemption (HDE), the timing for opening of the pilot cervical SCI study, and the company’s anticipated cash balance. Any forward-looking statements contained herein are based on current expectations, and are subject to a number of risks and uncertainties. Factors that could cause actual future results to differ materially from current expectations include, but are not limited to, risks and uncertainties relating to the company’s ability to successfully open additional clinical sites for enrollment and to enroll additional patients; the ability to complete the INSPIRE study and submit an HDE; the company’s ability to receive regulatory approval for the Neuro-Spinal Scaffold; the company’s ability to commercialize its products; the company’s ability to develop, market and sell products based on its technology; the expected benefits and efficacy of the company’s products and technology in connection with the treatment of spinal cord injuries; the availability of substantial additional funding for the company to continue its operations and to conduct research and development, clinical studies and future product commercialization; and other risks associated with the company’s business, research, product development, regulatory approval, marketing and distribution plans and strategies identified and described in more detail in the company’s Annual Report on Form 10-K for the year ended December 31, 2015, and its other filings with the SEC, including the company’s Form 10-Qs and current reports on Form 8-K. The company does not undertake to update these forward-looking statements.