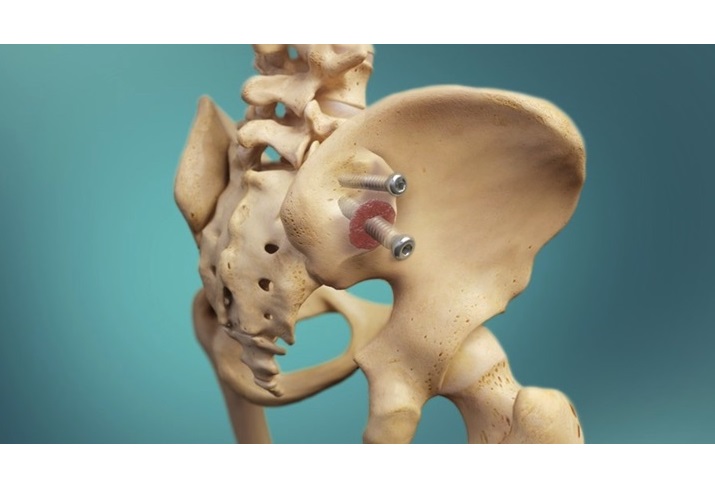
WARSAW, Ind., April 2, 2018 /PRNewswire/ — Zimmer Biomet Holdings, Inc. (NYSE and SIX: ZBH), a global leader in musculoskeletal healthcare, today announced the completion of the first surgical case utilizing its Comprehensive®Augmented Baseplate, which received FDA clearance on January 3, 2018. The case was performed by John W. Sperling, M.D., an orthopaedic surgeon at Mayo Clinic, who specializes in shoulder surgery. The Comprehensive Augmented Baseplate complements the Company’s Comprehensive® Reverse Shoulder System by offering an alternative to bone grafting and eccentric reaming for patients with glenoid defects undergoing shoulder reconstruction.
This newly cleared baseplate boasts a simplified circular design at three augment heights (3mm, 5mm and 7mm buildup), allowing for augment placement in any orientation to accommodate various unique bone anatomies. Its circular design also allows bone ingrowth into the rim of the baseplate for optimal fixation.
The Comprehensive Augmented Baseplate is a component of the Comprehensive Reverse Shoulder System, a next-generation reverse shoulder prosthesis engineered to offer high-quality intraoperative flexibility and clinically proven technologies. The system aims to minimize the potential challenges of removing well-fixed humeral stems by allowing conversion to a reverse shoulder using any of the existing Comprehensive stems. Additionally, the Comprehensive Augmented Baseplate leverages Mayo Clinic’s patented methodology for the optimization of shoulder arthroplasty components developed by Dr. Sperling at Mayo Clinic, Rochester, Minn., to provide relevant sizing for a conservative approach to bone removal in order to preserve bone stock if a future revision procedure is necessary.
“The new Augmented Baseplate rounds out Zimmer Biomet’s Comprehensive Shoulder portfolio and provides solutions that help surgeons with difficult glenoid deformity cases,” said Orsa Britton, Vice President and General Manager of Zimmer Biomet’s global Extremities business.
About Zimmer Biomet
Founded in 1927 and headquartered in Warsaw, Indiana, Zimmer Biomet is a global leader in musculoskeletal healthcare. We design, manufacture and market orthopaedic reconstructive products; sports medicine, biologics, extremities and trauma products; office based technologies; spine, craniomaxillofacial and thoracic products; dental implants; and related surgical products.
We collaborate with healthcare professionals around the globe to advance the pace of innovation. Our products and solutions help treat patients suffering from disorders of, or injuries to, bones, joints or supporting soft tissues. Together with healthcare professionals, we help millions of people live better lives.
We have operations in more than 25 countries around the world and sell products in more than 100 countries. For more information, visit www.zimmerbiomet.com, or follow Zimmer Biomet on Twitter at www.twitter.com/zimmerbiomet.
Cautionary Statement Regarding Forward-Looking Statements
This release contains forward-looking statements within the meaning of the safe harbor provisions of the Private Securities Litigation Reform Act of 1995. Forward-looking statements include, but are not limited to, statements concerning Zimmer Biomet’s expectations, plans, prospects, and product and service offerings, including new product launches and potential clinical successes. Such statements are based upon the current beliefs and expectations of management and are subject to significant risks, uncertainties and changes in circumstances that could cause actual outcomes and results to differ materially. For a list and description of some of such risks and uncertainties, see Zimmer Biomet’s periodic reports filed with the U.S. Securities and Exchange Commission (SEC). These factors should not be construed as exhaustive and should be read in conjunction with the other cautionary statements that are included in Zimmer Biomet’s filings with the SEC. Forward-looking statements speak only as of the date they are made, and Zimmer Biomet disclaims any intention or obligation to update or revise any forward-looking statements, whether as a result of new information, future events or otherwise. Readers of this release are cautioned not to rely on these forward-looking statements, since there can be no assurance that these forward-looking statements will prove to be accurate. This cautionary statement is applicable to all forward-looking statements contained in this release.
ZBH-Corp
SOURCE Zimmer Biomet Holdings, Inc.