DALLAS, February 20, 2018 /PRNewswire/ —
 FX Solutions, French number two in shoulder arthroplasty, has established an US subsidiary named FX Shoulder USA, Inc. to further expand directly into the US markets and to provide its current and future United State clients with an unique, large and innovative offer of shoulder implants.
FX Solutions, French number two in shoulder arthroplasty, has established an US subsidiary named FX Shoulder USA, Inc. to further expand directly into the US markets and to provide its current and future United State clients with an unique, large and innovative offer of shoulder implants.
FX Shoulder USA, based in Dallas, TX, was formed to proudly be the exclusive distributor for FX Solutions products effective January 1, 2018.
Created in 2011, FX Solutions has generated an annual growth of its turnover of more than 60% since its creation and plans to keep the same growth in 2018, particularly in the United States.
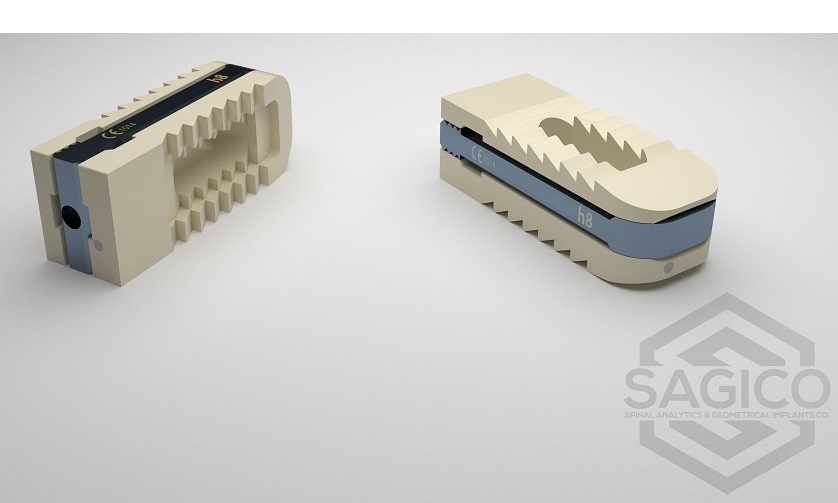
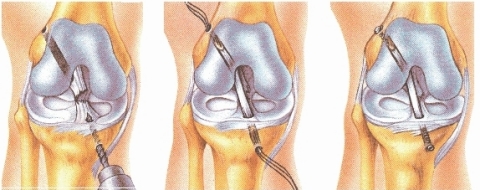
Its products have been approved in the USA since 2016 with the Humelock II, its only lockable shoulder trauma prosthesis available in the US. In January 2017, FX Solutions further expanded its portfolio with the introduction of the Humelock Reversed, a 145° reverse angle (available since 2011 in Europe). Additionally, in June 2017 it’s short stem Humeris was released as its primary platform.
FX Shoulder USA has quickly built a strong network of surgeons and distributors in Florida, Pennsylvania, Rhode Island, Maryland, Georgia and Texas and looks to further expand its distribution across the Midwest and West Coast. The group has strong growth ambitions and aims to develop rapidly in North America, the world’s largest market for shoulder prostheses.
FX Shoulder USA is the only company worldwide, and especially in the United States, to focus exclusively on shoulder arthroplasty. With a very technical and customer service-oriented approach, the company offers the best choice in shoulders replacement, adapted to any procedure the surgeon would require.
FX Shoulder USA will exhibit at the American Academy of Orthopedic Surgeons (AAOS) March 6-10, 2018 in New Orleans at booth n°3158 and at the American Shoulder and Elbow Surgeons (ASES) in Chicago in October 2018.
1-800-280-0775
info@fxshoulder.com
SOURCE FX Shoulder USA, Inc
(Photo: https://mma.prnewswire.com/media/643325/FX_Shoulder_USA_Humeris.jpg )