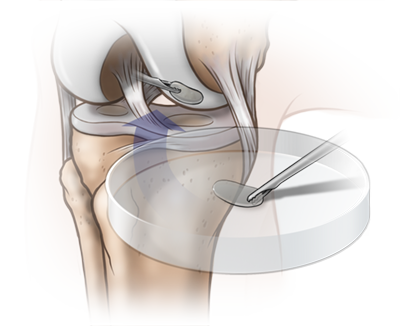
WALTHAM, Mass., May 08, 2017 (GLOBE NEWSWIRE) — Histogenics Corporation (Histogenics) (Nasdaq:HSGX), a regenerative medicine company focused on developing and commercializing products in the musculoskeletal space, today announced that it has successfully completed all formal consultations with the Office of Cellular and Tissue-based Products of the Japan Pharmaceuticals and Medical Devices Agency (the PMDA) regarding the Marketing and Manufacturing Authorization pathway for Histogenics’ NeoCart (autologous cell therapy designed to treat cartilage defects in the knee) in the Japanese market. Histogenics is currently nearing the completion of enrollment in a 245 patient Phase 3 clinical trial of NeoCart that is being conducted under a Special Protocol Assessment (the SPA) with the U.S. Food and Drug Administration (the FDA).
“We are very pleased with the formal feedback we received from the PMDA regarding the relatively expeditious approval pathway for NeoCart in Japan, and appreciate the thoughtful, rapid and collaborative approach provided by Japan regulators,” stated Adam Gridley, President and Chief Executive Officer of Histogenics. “These successful consultations and meetings are evidence of our execution of a broadening global regulatory strategy launched only seven months ago where we initiated efforts to leverage the robust U.S. clinical, preclinical and cGMP data for NeoCart into international markets. We believe the clarity on this efficient regulatory pathway for full Marketing Authorization will be important to our efforts to seek a development and commercialization partner for NeoCart in Japan and other markets in Asia.”
Various aspects of the Japanese regenerative medicine laws were updated in 2014 to potentially expedite the clinical development and commercialization pathways for innovative, qualified regenerative cell-based medicines that have demonstrated safety and probable efficacy. Shortly after reacquiring Japanese rights for NeoCart from Purpose Co. in May 2016, Histogenics initiated preparatory pre-consultations (Jizen-Mendan) with the PMDA for the three discreet modules of the regulatory process: Clinical Trial, Non-clinical Safety and Quality/Manufacturing.
During the first quarter of 2017, Histogenics held a series of consultations with the PMDA, including face-to-face (Taimen-Jogen) meetings. In these consultations, the PMDA agreed that Histogenics’ ongoing Phase 3 clinical trial with its one-year primary endpoint could be appropriate and provide sufficient evidence of safety and effectiveness for the full Marketing and Manufacturing Authorization in Japan. Furthermore, the PMDA agreed that a 30-patient, one-year confirmatory clinical trial in Japanese patients, comparing NeoCart to microfracture, would be sufficient for applying for full Marketing and Manufacturing Authorization in Japan. This Japanese study will utilize the same protocol as the ongoing Phase 3 clinical trial of NeoCart. Histogenics also confirmed that NeoCart would be regulated as a Regenerative Medical Product, as covered by the recently enacted laws in Japan, and that Histogenics’ current good manufacturing process (cGMP) in the U.S. could be utilized to manufacture and supply the confirmatory clinical study. These consultations with the PMDA were attended by representatives of Histogenics, including co-founder Dr. Shuichi Mizuno, regulatory and regenerative medicine experts, and two esteemed orthopedic surgeons from Japan, Dr. Akihiro Tsuchiya and Dr. Takumi Nakagawa, both of whom have trained on NeoCart procedures with U.S. surgeons.
In addition to the confirmatory clinical trial, Histogenics agreed with the PMDA to conduct additional minor, non-clinical safety studies, including a short-term (three-month) general toxicity study and in vitro tumorigenicity studies to reflect current standards and to augment the significant amount of pre-clinical data previously generated by Histogenics. These additional study protocols will be reviewed with the PMDA and will be conducted prior to the Marketing and Manufacturing Authorization. With regards to Histogenics’ Quality/Manufacturing applications, the PMDA and Histogenics agreed to several updates for certain procedures and testing methodology, all of which are planned as part of Histogenics’ continuous improvement activities for the biologics license application (BLA) submission planned with the FDA. Histogenics believes that the PMDA’s conclusions are based on the strength of the NeoCart clinical and non-clinical data package and the long 15+ year cGMP manufacturing history of NeoCart.
“We are thankful for the leadership and partnership with the PMDA,” commented Dr. Shuichi Mizuno, Ph.D., Co-founder of Histogenics, and Assistant Professor, Orthopedic Surgery, Brigham and Women’s Hospital, and Harvard Medical School. “We have been working collaboratively for nearly 20 years to provide substantial supportive basic science and non-clinical data as well as novel cell culture technology to guide the development of this important innovative therapy for cartilage defects.”
In conjunction with the launch of its commercial partnering efforts, Histogenics commissioned through Locust Walk’s Japan team a quantitative market research study with approximately 80 orthopedic surgeons including a mix of hospital physicians and general practitioners in Japan regarding the market opportunity for NeoCart for knee cartilage defects in the Japanese market. The findings paralleled what is observed from surgeons and patients in the United States – a market with a high unmet need characterized by long recoveries and variable clinical outcomes from current therapies, leaving many patients choosing to avoid having unsatisfactory treatments. These data may reflect the opportunity for innovative regenerative medicine products such as NeoCart to grow the market substantially by providing satisfactory outcomes and better quality of life, while avoiding progression to osteoarthritis (OA) and unnecessary surgeries.
The findings from the Japan survey include:
- Cartilage defects account for approximately 40% of total knee trauma cases causing pain and loss of function in the knee (with or without other injuries).
- Approximately 60% of patients with knee cartilage defects are either not treated at all, or treated only with conservative therapies (such as debridement) to temporarily treat pain.
- Approximately 60-70% of patients with knee cartilage defects that are left untreated will likely progress to OA, and 15-20% of their patients currently suffering from knee OA have such OA likely due to cartilage defects.
- More than 85% of orthopedic surgeons are not satisfied with the currently available treatment options for pain and loss of function due to knee cartilage defects.
- Approximately 80% of the surgeons consider early improvement in pain and function to be important and over half of the surgeons feel they would prescribe NeoCart based on the data already published.
“As is the case in the United States, we believe Japanese surgeons and patients are seeking new regenerative medicine options to repair cartilage defects that may offer both a more rapid recovery in terms of pain and function, as well as a more durable response over time with fewer repeat surgeries, which improves overall quality of life,” commented Dr. Tsuchiya, Vice President, Funabashi Orthopaedic Hospital, Chiba, Japan, and Chairman, Tokyo Women’s Medical College, Tokyo, Japan, and Dr. Nakagawa, Professor of Department of Orthopaedic Surgery, School of Medicine, Teikyo University, Tokyo, Japan. “We have followed the development of NeoCart for many years and have trained with surgeons in the U.S., and along with our medical colleagues, look forward to potentially introducing this novel non-NSAID and non-opioid cell-based therapy product to our patients in Japan that currently do not have good options to treat the pain and loss of function due to knee cartilage defects.”
Histogenics estimates the Japanese market represents a significant opportunity, with an estimated 200,000 procedures annually in Japan for patients suffering from pain associated with cartilage defects in the knee and limited options to treat the defect or related pain. If left untreated, cartilage defects may result in OA and ultimately, total knee replacements as patients age, with a substantial economic impact on patients and insurance companies. Market forecasts predict that the number of OA patients in Japan aged 40 and older amounts to more than 25 million and is expected to accelerate with the aging population. Once a development and commercial partner is identified, Histogenics intends to file with such partner the Clinical Trial Notification (CTN) to the PMDA to begin the proposed clinical trial.
About Histogenics Corporation
Histogenics is a leading regenerative medicine company developing and commercializing products in the musculoskeletal segment of the marketplace. Histogenics’ regenerative medicine platform combines expertise in cell processing, scaffolding, tissue engineering, bioadhesives and growth factors to provide solutions to treat musculoskeletal-related conditions. Histogenics’ first investigational product candidate, NeoCart is currently in Phase 3 clinical development. NeoCart is an autologous cell therapy designed to treat cartilage defects in the knee using the patient’s own cells. Knee cartilage defects represent a significant opportunity in the United States, with an estimated 500,000 or more applicable procedures each year. NeoCart is designed to exhibit characteristics of articular, hyaline cartilage prior to and upon implantation into the knee and therefore does not rely on the body to make new cartilage, characteristics not exhibited in other current treatment options. For more information, please visit www.histogenics.com.
Forward-Looking Statements
Various statements in this release are “forward-looking statements” under the securities laws. Words such as, but not limited to, “anticipate,” “believe,” “can,” “could,” “expect,” “estimate,” “design,” “goal,” “intend,” “may,” “might,” “objective,” “plan,” “predict,” “project,” “target,” “likely,” “should,” “will,” and “would,” or the negative of these terms and similar expressions or words, identify forward-looking statements. Forward-looking statements are based upon current expectations that involve risks, changes in circumstances, assumptions and uncertainties.
Important factors that could cause actual results to differ materially from those reflected in Histogenics’ forward-looking statements include, among others: the timing and success of Histogenics’ NeoCart Phase 3 clinical trial; possible delays in enrolling the NeoCart Phase 3 clinical trial; the ability to obtain and maintain regulatory approval of NeoCart or any product candidates in the U.S. and Japan, and the labeling for any approved products; Histogenics’ ability to find a development and commercialization partner for NeoCart in Japan; the scope, progress, expansion, and costs of developing and commercializing Histogenics’ product candidates; the ability to obtain and maintain regulatory approval regarding the comparability of critical NeoCart raw materials; the size and growth of the potential markets for Histogenics’ product candidates and the ability to serve those markets; Histogenics’ expectations regarding its expenses and revenue; the sufficiency of Histogenics’ cash resources and the availability of additional financing on commercially reasonable terms; the early stage of development of the technologies on which Histogenics’ channel partnering agreement with Intrexon is based; the additional expenses that Histogenics may incur in connection with its exclusive channel collaboration agreement with Intrexon Corporation and other factors that are described in the “Risk Factors” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations” sections of Histogenics’ Annual Report on Form 10-K for the year ended December 31, 2016, which is on file with the SEC and available on the SEC’s website at www.sec.gov. Additional factors may be set forth in those sections of Histogenics’ Quarterly Report on Form 10-Q for the quarter ended March 31, 2017, to be filed with the SEC in the second quarter of 2017. In addition to the risks described above and in Histogenics’ annual report on Form 10-K and quarterly reports on Form 10-Q, current reports on Form 8-K and other filings with the SEC, other unknown or unpredictable factors also could affect Histogenics’ results.
There can be no assurance that the actual results or developments anticipated by Histogenics will be realized or, even if substantially realized, that they will have the expected consequences to, or effects on, Histogenics. Therefore, no assurance can be given that the outcomes stated in such forward-looking statements and estimates will be achieved.
All written and verbal forward-looking statements attributable to Histogenics or any person acting on its behalf are expressly qualified in their entirety by the cautionary statements contained or referred to herein. Histogenics cautions investors not to rely too heavily on the forward-looking statements Histogenics makes or that are made on its behalf. The information in this release is provided only as of the date of this release, and Histogenics undertakes no obligation, and specifically declines any obligation, to update or revise publicly any forward-looking statements, whether as a result of new information, future events or otherwise.
Contact:
Investor Relations
Tel: +1 (781) 547-7909
InvestorRelations@histogenics.com

Source: Histogenics Corporation
Read more: http://www.nasdaq.com/press-release/histogenics-announces-agreement-with-the-japan-pharmaceuticals-and-medical-devices-agency-regardin-20170508-00226#ixzz4gVichFvl