November 30, 2018
DUBLIN–(BUSINESS WIRE)–The “Global Hip & Knee Reconstruction Devices Market Analysis & Trends – Industry Forecast to 2027” report has been added to ResearchAndMarkets.com’s offering.
The Global Hip & Knee Reconstruction Devices Market is poised to grow strong during the forecast period 2017 to 2027.
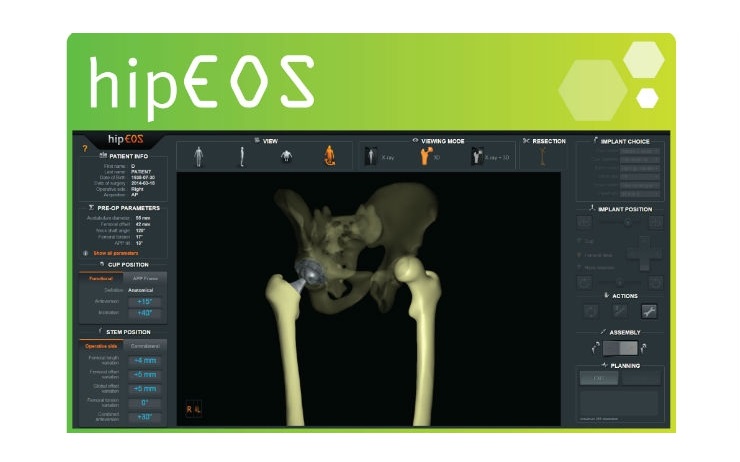
Some of the prominent trends that the market is witnessing include rising gap between hospital costs and reimbursements, computer-assisted total hip replacement surgery is one of the hottest revolutions and latest technological developments of hip & knee reconstruction devices.
This industry report analyzes the market estimates and forecasts of all the given segments on global as well as regional levels presented in the research scope. The study provides historical market data for 2015, 2016 revenue estimations are presented for 2017 and forecasts from 2018 till 2027.
The study focuses on market trends, leading players, supply chain trends, technological innovations, key developments, and future strategies. With comprehensive market assessment across the major geographies such as North America, Europe, Asia Pacific, Middle East, Latin America and Rest of the world the report is a valuable asset for the existing players, new entrants and the future investors.
The study presents detailed market analysis with inputs derived from industry professionals across the value chain. A special focus has been made on 23 countries such as U.S., Canada, Mexico, U.K., Germany, Spain, France, Italy, China, Brazil, Saudi Arabia, South Africa, etc.
The market data is gathered from extensive primary interviews and secondary research. The market size is calculated based on the revenue generated through sales from all the given segments and sub segments in the research scope. The market sizing analysis includes both top-down and bottom-up approaches for data validation and accuracy measures.
Report Highlights
- The report provides a detailed analysis on current and future market trends to identify the investment opportunities
- Market forecasts till 2027, using estimated market values as the base numbers
- Key market trends across the business segments, Regions and Countries
- Key developments and strategies observed in the market
- Market Dynamics such as Drivers, Restraints, Opportunities and other trends
- In-depth company profiles of key players and upcoming prominent players
- Growth prospects among the emerging nations through 2027
- Market opportunities and recommendations for new investments
Key Topics Covered
1 Market Outline
1.1 Research Methodology
1.1.1 Research Approach & Sources
1.2 Market Trends
1.3 Regulatory Factors
1.4 Product Analysis
1.5 Strategic Benchmarking
1.6 Opportunity Analysis
2 Executive Summary
3 Market Overview
3.1 Current Trends
3.1.1 Rising gap between hospital costs and reimbursements
3.1.2 Computer-assisted total hip replacement surgery is one of the hottest revolutions
3.1.3 Latest Technological Developments of Hip & Knee Reconstruction Devices
3.1.4 Growth Opportunities/Investment Opportunities
3.2 Drivers
3.3 Constraints
3.4 Industry Attractiveness
3.4.1 Bargaining power of suppliers
3.4.2 Bargaining power of buyers
3.4.3 Threat of substitutes
3.4.4 Threat of new entrants
3.4.5 Competitive rivalry
4 Hip & Knee Reconstruction Devices Market, By Product
4.1 Knee Reconstruction Devices
4.1.1 Partial Knee Reconstruction Devices
4.1.2 Primary Cemented Knee Reconstruction Devices
4.1.3 Revision Knee Reconstruction Devices
4.1.4 Primary Knee Reconstruction Devices
4.1.5 Primary Cementless Knee Reconstruction Devices
4.2 Hip Reconstruction Devices
4.2.1 Partial Hip Reconstruction Devices
4.2.2 Hip Resurfacing Devices
4.2.3 Primary Hip Reconstruction Devices
4.2.4 Revision Hip Reconstruction Devices
5 Hip & Knee Reconstruction Devices Market, By Geography
5.1 North America
5.2 Europe
5.3 Asia Pacific
5.4 Middle East
5.5 Latin America
5.6 Rest of the World (RoW)
6 Key Player Activities
6.1 Acquisitions & Mergers
6.2 Agreements, Partnerships, Collaborations and Joint Ventures
6.3 Product Launch & Expansions
6.4 Other Activities
7 Leading Companies
7.1 Stryker Corporation
7.2 Corentec
7.3 Zimmer Biomet
7.4 Smith & Nephew PLC
7.5 Arthrex, Inc.
7.6 United Orthopedics Corporation
7.7 Baumer S.A.
7.8 Beijing Chunlizhengda Medical Instruments Co. Ltd.
7.9 DJO Global
7.10 Exactech, Inc.
7.11 Tornier, Inc
7.12 Allegra Orthopaedics Limited
7.13 Corin Group PLC
7.14 Japan MDM, Inc.
7.15 DePuy Synthes
For more information about this report visit https://www.researchandmarkets.com/research/2rknvs/global_hip_and?w=4
Contacts
ResearchAndMarkets.com
Laura Wood, Senior Press Manager
press@researchandmarkets.com
For E.S.T Office Hours Call 1-917-300-0470
For U.S./CAN Toll Free Call 1-800-526-8630
For GMT Office Hours Call +353-1-416-8900
Related Topics: Orthopedic Devices