September 12, 2016
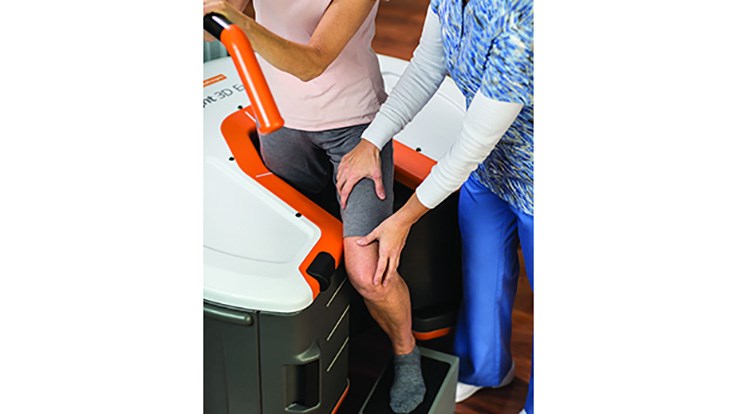
LEWISVILLE, Texas–(BUSINESS WIRE)–Orthofix International N.V., (NASDAQ:OFIX), a diversified, global medical device company, today announced enrollment of the first patient in a study evaluating the use of pulsed electromagnetic field (PEMF) technology for osteoarthritis (OA) of the knee. This study will assess the efficacy and safety of the Company’s Physio-Stim system in reducing inflammation and restoring homeostasis of the extracellular matrix, potentially providing symptomatic relief of OA pain, reducing cartilage breakdown and stimulating new cartilage formation. If successful, this would be the first disease-modifying treatment for osteoarthritis. Preservation or restoration of joint structure together with reduction of inflammation would be expected to improve symptoms and reduce the need for surgical intervention.
The first patient in the study was enrolled by Dr. Roy Aaron, Professor at Brown University in Providence, RI. “Finding new solutions for OA of the knee is important as these patients not only suffer from pain, they often have a high level of disability from the disease and often seek costly surgical solutions,” said Dr. Aaron. “We are hopeful that active PEMF stimulation may provide us with a new non-invasive treatment approach that could help patients with knee OA avoid surgery and improve their overall quality of life.”
The OA of the knee study is a prospective, randomized, double-blind, placebo-controlled feasibility trial that will enroll approximately 150 patients who are 40 years of age or older at three sites in the U.S. These include Brown University School of Medicine in Providence, RI; Sinai Hospital of Baltimore in Baltimore, MD; and the Cleveland Clinic in Cleveland, OH. Study participants will be randomized in a two-to-one ratio to either an active or placebo control (inactive) device and followed for 12 months after initiation of treatment.
“This study demonstrates Orthofix’s vision of developing new applications for our PEMF technology,” said James Ryaby, Ph.D., Chief Scientific Officer for Orthofix. “We are proud to conduct research studies like these in order to find solutions for patients who live with disabling diseases and conditions such as OA.”
The Orthofix Physio-Stim device is currently approved by the U.S. Food and Drug Administration (FDA) for the treatment of nonunion fractures. The device uses a low-level electromagnetic field (PEMF) that helps activate and augment the body’s natural healing process. Use in the OA study is investigational and is being conducted under an Investigational Device Exemption (IDE) from the FDA. More information is available at ClinicalTrials.gov.
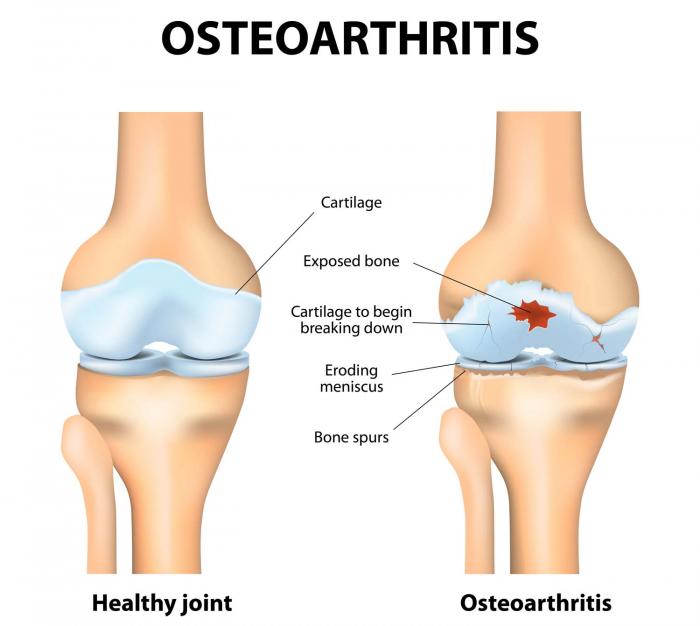
About Osteoarthritis of the Knee
Osteoarthritis is a common disease and one of the leading causes of disability. The Centers for Disease Control and Prevention estimate that nearly one in two people may develop symptomatic knee OA by age 85. Statistics show that in 2011 alone, there were 757,000 total knee replacement procedures performed, with OA accounting for 95 percent of these surgeries. Osteoarthritis of the knee is a degenerative, “wear-and-tear” type of arthritis where the cartilage in the knee joint gradually wears away. This painful disease most often effects people 50 years of age and older, but may occur in younger people, too. People with OA of the knee often experience pain when walking, running, bending or kneeling. They may also experience joint stiffness and swelling, making it difficult to do many everyday activities.
About Orthofix
Orthofix International N.V. is a diversified, global medical device company focused on improving patients’ lives by providing superior reconstructive and regenerative orthopedic and spine solutions to physicians worldwide. Headquartered in Lewisville, TX, the company has four strategic business units that include BioStim, Biologics, Extremity Fixation and Spine Fixation. Orthofix products are widely distributed via the company’s sales representatives, distributors and subsidiaries. In addition, Orthofix is collaborating on research and development activities with leading clinical organizations such as Brown University, Sinai Hospital of Baltimore, Cleveland Clinic, Texas Scottish Rite Hospital for Children and the Musculoskeletal Transplant Foundation. For more information, please visit www.orthofix.com.
Forward-Looking Statements
This communication contains certain forward-looking statements under the Private Securities Litigation Reform Act of 1995. These forward-looking statements, which may include, but are not limited to, statements concerning the projections, financial condition, results of operations and businesses of Orthofix and its subsidiaries, are based on management’s current expectations and estimates and involve risks and uncertainties that could cause actual results or outcomes to differ materially from those contemplated by the forward-looking statements. The forward-looking statements in this release do not constitute guarantees or promises of future performance. Factors that could cause or contribute to such differences may include, but are not limited to the risks described in the “Risk Factors” section of our 2015 Annual Report on Form 10-K, as well as in other reports that we file in the future. Existing and prospective investors are cautioned not to place undue reliance on these forward-looking statements, which speak only as of the date hereof. The Company undertakes no obligation to update or revise the information contained in this press release.
Contacts
Orthofix International N.V.
Investor Relations
Mark Quick, 214-937-2924
markquick@orthofix.com
or
Media Relations
Denise Landry, 214-937-2529
deniselandry@orthofix.com