OAKLAND, N.J., Nov. 22, 2016 /PRNewswire/ — Collagen Matrix, Inc., which advances the science of tissue repair and regeneration by designing, developing and manufacturing collagen and mineral based medical devices that support the body’s natural ability to regenerate, announced today the appointment of Oystein Valberg as its Chief Financial Officer. Mr. Valberg will oversee finance and administration as well as the human resources team.
Mr. Valberg has more than 20 years of progressive senior corporate finance leadership and business development experience, including 17 years with Medtronic Plc where he earned a reputation as a strong, “hands on” organizational leader.
Most recently, he served as CFO and Vice President of Finance, Strategy and Business Development for Medtronic’s Surgical Technology business unit. His valuable experience working with Medtronic also included responsibilities in Corporate Development, Treasury and Investor Relations.
Prior to Mr. Valberg’s tenure at Medtronic, he served as an Analyst with US Bankcorp, and as an Auditor for Grant Thornton where he earned his CPA. Mr. Valberg earned a bachelor’s degree and a master’s degree in business administration from the Carlson School of Management in Minneapolis.
Bart Doedens, Collagen Matrix CEO, commented: “We are excited and pleased to welcome Oystein to our executive team. As we continue to build our framework for growth, Oystein will be one of the contributors to our success. His background and experience are an excellent fit and will serve us well.”
About Collagen Matrix
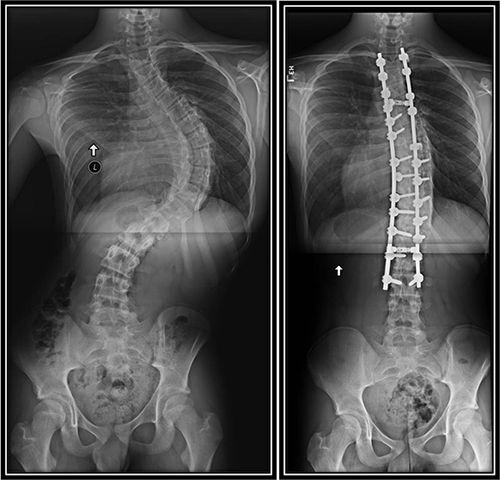
Collagen Matrix, Inc., founded in 1997, delivers a full line of the highest-quality collagen and mineral based medical devices that support the body’s natural ability to regenerate. The Company currently manufactures finished medical devices in the areas of Dental, Neurosurgical, Spine, Orthopaedic and Nerve Repair Surgery. More information about Collagen Matrix can be found at www.collagenmatrix.com.
Contact:
Margo Lane
201-405-1477
mlane@collagenmatrix.com
Photo – http://photos.prnewswire.com/prnh/20161122/442064
To view the original version on PR Newswire, visit:http://www.prnewswire.com/news-releases/collagen-matrix-inc-names-oystein-valberg-as-chief-financial-officer-300367468.html