For patients that seek treatment from physical therapists, the prospect of achieving faster and better results when rehabbing from injury or receiving treatment for pain is a no-brainer.
For patients that seek treatment from physical therapists, the prospect of achieving faster and better results when rehabbing from injury or receiving treatment for pain is a no-brainer.
Now, with an increasing number of physical therapy clinics incorporating in-house diagnostics into the practice this is not only possible, but expected.
Armed with more objective results from established tests that include nerve conduction, musculoskeletal ultrasound and other tests, physical therapists are now able to troubleshoot issues with challenging patients much more quickly and accurately in the clinic.
As a result, patients are able to get back to work sooner, return to their beloved sports/exercises and even potentially lead a more pain-free existence without medication.
The traditional approach to PT
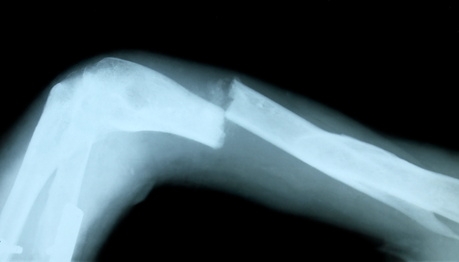
In the traditional approach, physical therapists evaluate patients through a physical examination to determine the ideal treatment plan. However, Physical Therapy physical evaluation tests may miss pathologies and lead to ineffective treatment.
“As physical therapists, a lot of what we do is relatively subjective testing,” explains Nathan Shields, co-owner of Rise Rehabilitation Specialists with 18 years as an orthopedic physical therapist. “Many of the tests are scientifically proven, but are still based upon the skill level and experience of the therapist.”
In the past, when more sophisticated diagnostic tests were required the patient was typically referred to a small universe of specialists in a process that could take several weeks to receive the results.
Now, however, PTs are regularly bringing this type of testing into the clinic. This not only requires a significant investment in the equipment, but also training to accurately conduct the tests.
Fortunately, this is being facilitated by national franchise organizations such as Hands-On Diagnostics that help physical therapy practices establish in-house diagnostic services. To date, the franchise has expanded to 18 different states with over 115 physical therapy facilities.
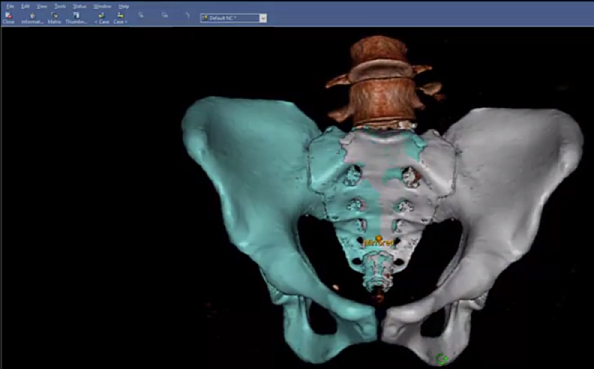
Among the tests that physical therapists can be trained on include electromyography (EMG), Nerve Conduction Studies (NCS), musculoskeletal and neuro ultrasound, vestibular testing to evaluate patients with vertigo and balance problems and Evoked Potential tests.
EMG/NCS testing is one of the most reliable diagnostic tools for many dysfunctions of the Neuromuscular System. An EMG measures the electrical activity of muscles at rest and during contraction. Nerve Conduction Studies (NCS) measure the health of the nerves.
Physical therapists have been able to perform EMG and nerve conduction tests for more than 45 years. In 1978, the American Physical Therapy Association established a specialty program through the American Board of Physical Therapist Specialties for certification in clinical electrophysiology.
The other diagnostic technique is Musculoskeletal Ultrasound (MSKUS) imaging, which uses sound waves to produce pictures of muscles, tendons, ligaments and joints throughout the body. It is used to help diagnose sprains, strains, tears, and other soft tissue conditions and to guide therapeutic procedures.
In addition to identifying the severity of the problem, EMG and MSKUS can be used to locate the actual source of pain conditions as well as to monitor ongoing improvement over the course of the physical therapy treatment plan.
Patient Feedback
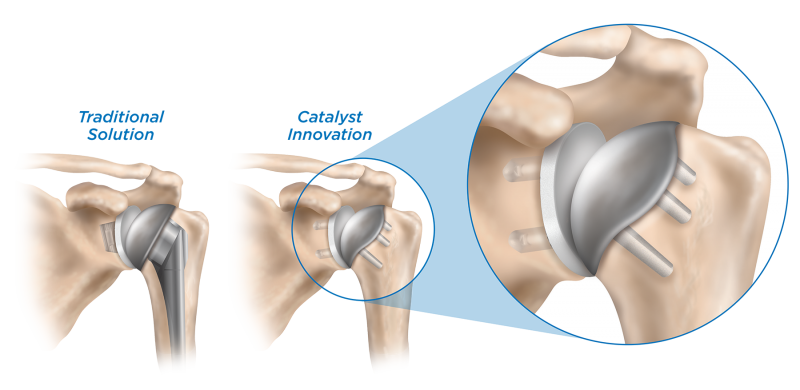
According to a September 27, 2017 article in Musculoskeletal Care, “Physiotherapists utilizing diagnostic ultrasound in shoulder clinics. How useful do patients find immediate feedback from the scan as part of the management of their problem?” the utilization of diagnostic ultrasound by physical therapists in patients with shoulder problems concluded that patients highly rated the information gained from ultrasound imaging in a physical therapy environment and felt it assisted them in the understanding, reassurance and management of their problem.
According to the article, to arrive at this conclusion a questionnaire was offered to 103 patients that underwent ultrasound imaging as part of a shoulder assessment over a 6-month period.
According to the article, “Regarding the ability to understand their shoulder problem better and in feeling reassured about their problem, 97% of patients either strongly agreed or agreed that this was the case. Concerning the capability of managing their problem, 89% of patients strongly agreed or agreed that they felt more able to do this. In total, 96% of patients evaluated the ultrasound scan to be of very high/high value to them.”
For Physical Therapist Nathan Shields, perhaps the most important aspect is that patients are experiencing better, faster results.
“We are now able to treat patients with more certainty and, in some cases, we have been able to use the testing to create protocols and get immediate responses on the physical therapy side,” says Shields.
For more information, contact Hands-On Diagnostics at (888) 447-6014 or visit www.diagnosticsforpt.com